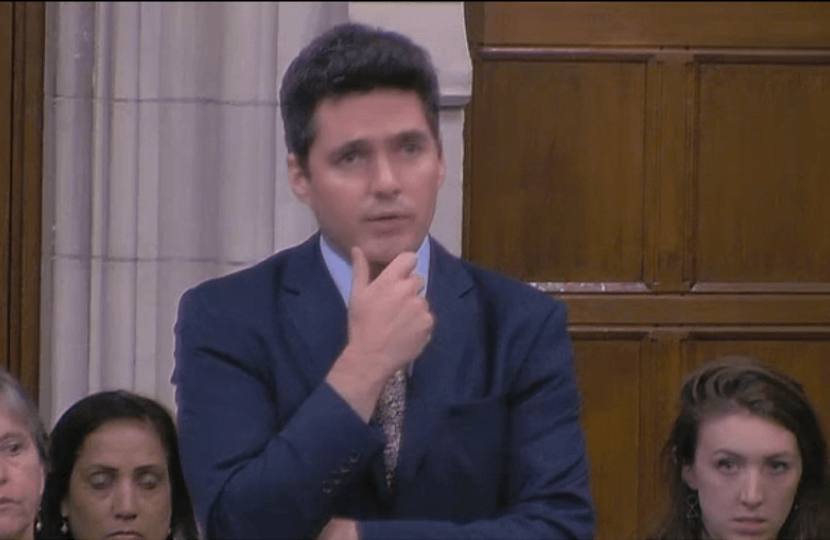
Huw spoke about the future of breast cancer in a debate. He paid tribute to those living with the disease and those caring for them. He also spoke of some of the issues facing those going through treatment, including challenges in the NHS communications system, vowing to fight to make the situation better through his work in parliament.
Video here: https://goo.gl/ZppwNj
Full Speech:
"It is a pleasure to serve under your chairmanship, Mr McCabe. I thank the hon. Member for Crewe and Nantwich (Laura Smith) for leading the debate with such care, passion and expertise. It is a great pleasure to note that the three Front-Bench spokespeople—the Under-Secretary of State for Health and Social Care, my hon. Friend the Member for Winchester (Steve Brine), the hon. Member for Washington and Sunderland West (Mrs Hodgson) and the hon. Member for Central Ayrshire (Dr Whitford) —have all served as chairs of the all-party parliamentary group on breast cancer. It is a rarity for all three Front-Bench spokespeople to have so much knowledge and, indeed, to care so much about the issue that they have spent their time campaigning on it in Parliament. I salute all three of them for their work on this matter and I very much look forward their contributions.
The statistics are well known and well rehearsed, but I want to put them on record. In the UK, 55,000 women and 350 men are diagnosed with breast cancer every year. Sadly, one in eight women will be diagnosed with breast cancer, 35,000 women are living with secondary breast cancer, and nearly 1,000 women die from breast cancer every month. Nearly 700,000 people in the UK are living either with or beyond breast cancer treatment. The positive that we can look at now is that 80% of women survive for five years or more. The title of the debate on the Order Paper, “Future of breast cancer”, is crucial, because it is all about the future. The progress made so far has been absolutely extraordinary, but we must not rest on that progress; we must look further forward and do even more, as science and medical developments allow us to.
I would probably have trotted out those statistics a couple of years ago when speaking on this matter, because it impacts on my constituents. However, personal experience of a loved one being struck down with breast cancer makes me more determined to be here to represent their cause and that of the thousands of women across the country who have to go through the same experience. I salute the courage and bravery of all who have been diagnosed with breast cancer and who have gone through the treatment. To watch those people undertake that brave journey is a humbling experience, because when I saw it with my own eyes, I thought, “Could I actually do this? Would I have the bravery and the strength to go through this myself?” It was the most extraordinary experience for me to see that.
I pay tribute to all the carers and those who provide support. They feel helpless, at times, and they wish that they could go through the wretched experience instead. They would do anything to change places, but they cannot. Those people do the most amazing job. On behalf of those who have been through the treatment, I salute all the brave families, friends and loved ones who went through it with them. The inner strength that their support must give to sufferers is absolutely tremendous.
Breast screening uptake is at its lowest level for 10 years, which is very concerning. Uptake is at 71%; the aim is to make that figure at least 80%, which would save 1,200 lives per year. If the Minister has time, I would like him to reassure us that the Government will take action in their attempt to reach that target. Screening is, of course, still age-based, and it was sad for me to note that the entry-level screening age would have been too high for the family member I referred to, who was only 42 when they were diagnosed.
It is incredibly exciting to meet groups such as Breast Cancer Now, which is carrying out a generation study, following 113,000 women from the UK over 40 years. I was absolutely blessed and fascinated to meet the people involved in that study at a recent all-party parliamentary group meeting. Of course, age is one profile, but we need to look at high-risk scenarios and investigate the genetic, lifestyle and environmental factors that can change the likelihood of a woman developing breast cancer. That study, which I think is exciting, identifies 160 common genetic changes associated with the development of breast cancer, as well as showing how various life events—such as the menopause—and lifestyle factors can have a great impact. The future is bright, because rather than just looking at age ranges, we are now really going into the detail with those studies to show how certain factors can lead to risk and then, where there is risk, providing screening. That is hugely important.
I paid tribute to those who go through breast cancer treatment and to their carers, who go through it with them, but I also want to touch on the phenomenal work that NHS staff do for everyone who goes through that journey. I thank them; they are the most extraordinary people, in terms of their sheer intelligence. It is incredibly reassuring to meet such bright, dedicated people. The other great thing about them is that they deal with everything in black and white—there is no messing around—and tell people exactly what is going on. It can sometimes be stark, but it reassures people that they are being led to the right conclusion.
Of course, there are workload impacts. We know that the NHS faces challenges, and cancer departments absolutely share those challenges. A Macmillan Cancer Support survey from last year highlighted the increased workloads, complex patient needs and vacancies in key roles that are putting pressure on the cancer care workforce. Certainly, in my experience with the Maidstone and Tunbridge Wells NHS Trust, the staff were absolutely phenomenal. When things did not work, it was often because they did not have what is called back-office support. As a result, consultants have to run around doing admin work instead of focusing on their medical and clinical expertise, making them very expensive and overqualified admin resources. We often talk quite clinically about back-office savings, but perhaps we need to look very carefully before making such savings if they will have an impact on frontline services.
Some of the NHS communications systems can be incredibly clunky. Finding out via Royal Mail that one has an appointment after the appointment is due to take place—not just once, but twice—is maddening. These days, we embrace technology. We are told about dentist appointments via text messages to which we can respond to confirm, and the NHS should be doing the same thing. Before my journey with breast cancer, I was critical of people who missed appointments, but I had not reflected that people might miss appointments because they have not been told that they are taking place. It is maddening for consultants, because once people have received their notification, they are not even required to reply to confirm that they will attend their appointment. Of course, no one in the hospital thinks, “Someone has not got back to me; perhaps they have not received the letter.” We sat waiting in the hospital for hours, because the system did not know we were there despite the fact that we had booked in. That is maddening for patients, and maddening for consultants and staff.
Such issues may seem quite trivial, but they caused me to go back to the hospital to meet the heads of service to ensure that I could convey the concerns of frontline staff to senior management. I thought that that was the least I could do after the care and attention that the staff had given us.
I therefore ask my hon. Friend the Minister to think about the support staff, the systems that are in place and how we can better support the staff who help us to get better. I express my immense gratitude for those people and the support, expertise and help that they provide, not just during the treatment but on the journey beyond. That is the other thing that I have noticed: once a patient is given the all-clear, which is the best news, all of a sudden they face another journey, on which they will not necessarily be with clinicians. They will still have support staff from organisations such as Macmillan, who take great care of people.
I find myself speaking from experience, having been on an incredible journey that taught me a great deal about those who go through cancer and those who care for us through cancer. It has made me vow that I will always do everything I can in Parliament to try to make the situation better. I look forward to those on the Front Benches reassuring us that they will do the same."


